Females and Young Adults at Higher Risk of COVID-19 Vaccine Side Effects: Study

The authors also found different side effects were linked with different doses.
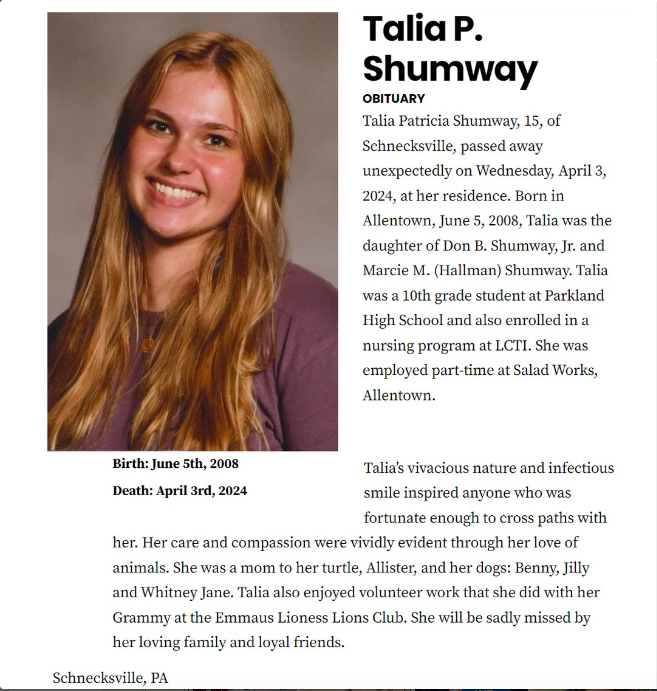
Females and young adults are more likely to experience side effects following COVID-19 vaccinations. A Japanese study discovered that people who take three doses as opposed to two may experience different side effects.
The study, which was published in November in Scientific Reports, followed 272 hospital employees who received the Pfizer vaccine as a second dose between January and June 2022.
There was no prior history of COVID-19 infection among the participants, and all of their symptoms were examined and diagnosed by hospital doctors.
The researchers discovered “higher frequencies of COVID-19 vaccine-related side effects” and “worse outcomes with longer recovery from side effects” in females and younger adults versus males and elderly adults.
Third Dose Versus Second Dose
The authors discovered that different doses were associated with different side effects, with the side effects after the third dose being more long-lasting and severe than the side effects after the second dose.
Axillary pain is much more common in people who have taken three doses rather than two. Headaches and joint pain are common side effects that tend to last longer after the third dose than the second or first dose.
Common side effects of the second dose include asthma symptoms, ear fullness, numbness in the upper arm, and injection at the injection site.
The author linked symptoms after the second vaccine dose to an allergic reaction, while headaches and joint pains after the third dose were linked to inflammation and immune dysregulation.
Health Practitioners Report Similar Findings
Doctors and other studies have found similar demographics in patients who report post-vaccination symptoms.
According to REACT19’s 2022 post-vaccine survey, females, particularly those aged 30 to 50, are at a higher risk of symptoms following vaccination.
Additional vaccines also have a cumulative effect, so people who have had more shots are at a higher risk of worse symptoms, according to internist Dr. Keith Berkowitz, who has treated over 200 long COVID and post-vaccine patients.
According to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report, the majority of people who report anaphylaxis are female.
A JAMA Network Open study found that females were more likely to report adverse effects from Moderna and Pfizer vaccinations. The study’s authors reasoned that females produced more antibodies after vaccination, and that higher levels of estrogen and progesterone in females may result in different symptom manifestations.
Younger people also have a stronger immune system, and the patient’s side effects could be due to the immune response, the authors reasoned.
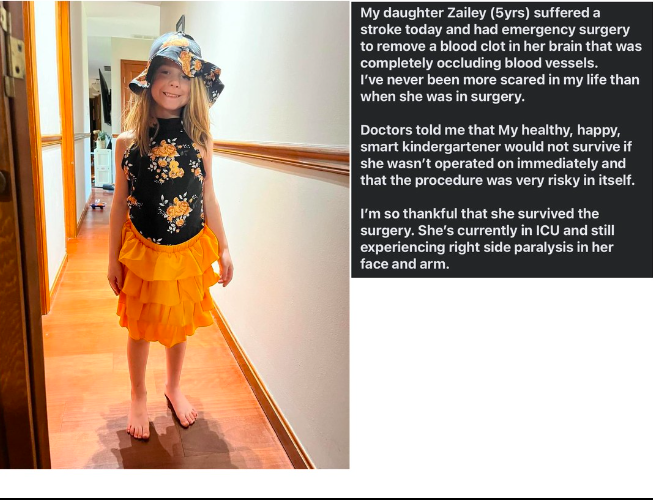
The COVID-19 mRNA vaccines stimulate the body’s production of spike proteins. These spike proteins have the potential to cause blood vessel damage, clotting, inflammation, and even autoimmunity. Greater symptom severity indicates more reactive symptoms caused by the body’s attempts to combat the spike proteins.
While this may aid in the removal of spike proteins, it may also impede recovery by directing the body’s resources toward fighting an infection rather than resting and recovering. “If the immune system is functioning better … the body functions better as a whole and the body can use its needed sources elsewhere,” said Dr. Berkowitz.
Changing Demographics
Leading Edge Clinic nurse practitioner Scott Marsland told The Epoch Times that he has noticed a shift in his patient population in recent months.
“I have a lot more male patients these days and … we’re getting more patients who have had multiple vaccinations and boosters,” Mr. Marsland told the audience. Many patients are now referred by friends and family members who believe they are suffering from vaccine side effects. These people are more skeptical and distrusting because they haven’t been following the research on COVID-19 vaccine injuries, he says.
Dr. Berkowitz added that as the pandemic progressed, he began to see a variety of patients, the majority of whom had multiple COVID-19 infections and had received multiple doses of the COVID-19 vaccine. Because each infection and injection increases the load of spike protein, Dr. Keith says, “I’ll list how many times they’ve had the vaccine and how many times they’ve been infected [to assess treatment].”