Unprecedented Surges in Cardiac Arrest Cases in Victoria, Australia: Exploring the Potential Vaccine Link

Research has established a causal relationship between vaccines and myocarditis—a common cause of sudden cardiac arrest in young individuals.
There has been a significant increase in the number of cardiac arrest cases in Victoria, Australia, over the last two years. Cases increased by 5.8 percent from 2021 to 2022 compared to the previous year, reaching a new high. These figures have sparked public concern about potential vaccine side effects.
According to the Victorian Ambulance Cardiac Arrest Registry’s annual report, 6,934 cases were recorded from 2020 to 2021, representing a 2.5 percent increase over the previous year and the highest number of cardiac arrest events in the state at the time. However, in just one year, from 2021 to 2022, the number of cases increased to 7,361 incidents, a new historical high.
Is There a Connection Between Cardiac Arrest and Vaccination?
Numerous large-scale studies show that myocarditis is the leading cause of sudden and unexpected death in adults under the age of 40. The rising prevalence of myocarditis in young people may increase the risk of other serious cardiovascular events, such as cardiac arrest and acute coronary syndromes.
According to CovidBaseAU, an Australian COVID-19 vaccine tracking website, as of September 1, 2023, 97.53 percent of people aged 16 and up in the country had received at least one dose of the vaccine.
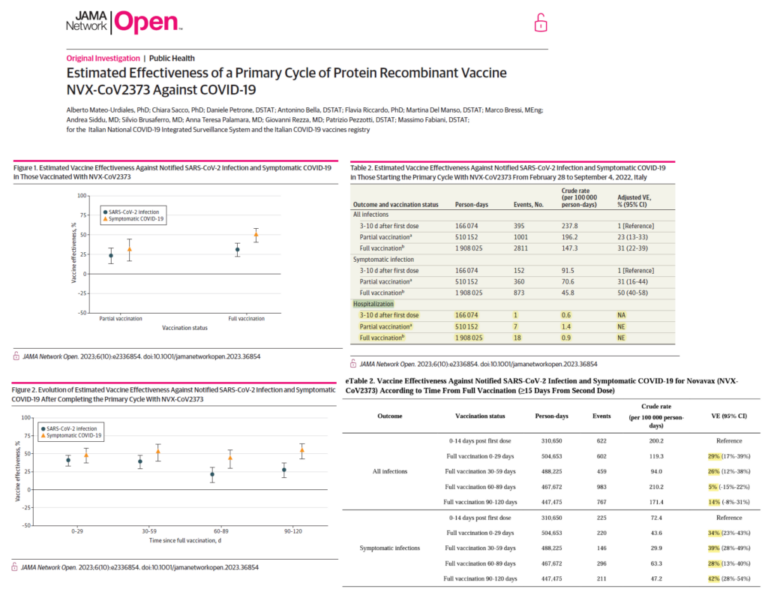
Myocarditis and pericarditis have been linked to mRNA vaccines and the Nuvaxovid (Novavax) vaccine, according to the Australian government. Per 100,000 doses of Nuvaxovid vaccination, there are approximately 3 to 4 reported cases of myocarditis and 13 reported cases of pericarditis. Males aged 18 to 49 are more likely to develop pericarditis, with an estimated 27 cases per 100,000 doses. According to the government, myocarditis is a known but extremely rare side effect of mRNA vaccines.
However, according to a study published in May of this year, myocarditis (with an overall incidence rate of around 1.62 percent) is the most common cardiac event following COVID-19 vaccination. It has been reported that cases of myocarditis are more common in men and after the second dose. Furthermore, when compared to inactivated vaccines, the use of mRNA and vector-based vaccines is associated with a higher incidence of vaccine-induced thrombotic thrombocytopenia and pulmonary embolism.
According to other studies, the incidence of post-COVID-19 vaccination heart cases is low, and they are mostly of mild severity. If the second vaccine dose is given more than 30 days after the first, the risk of developing myocarditis or pericarditis may be reduced.
Dr. Eli Jaffe, a leading figure in emergency medicine and health care management in Israel, and colleagues published a startling study in the journal Scientific Reports in 2022. The researchers examined data from Israel’s National Emergency Medical Services, which revealed that there was a more than 25% increase in emergency calls related to cardiac arrest and acute coronary syndrome (a severe form of coronary heart disease) among people aged 16 to 39 from January to May 2021, compared to the same period in 2019 and 2020.
The researchers discovered that the increase in emergency calls for cardiac issues was related to the administration of the COVID-19 vaccine but unrelated to COVID-19 infection.
The study’s authors stated that the findings have raised concerns about vaccine-induced severe cardiovascular side effects that have gone undetected. They emphasized the well-established link between vaccines and myocarditis, which is a common cause of sudden cardiac arrest in young people.
The findings are consistent with adverse event reporting systems and clinical evidence from other countries, emphasizing the presence of a wide range of side effects associated with COVID-19 vaccines, some of which can be severe.
Another Israeli study found that, when compared to the expected incidence rate based on historical data, the rate of myocarditis in young males (aged 16 to 19) increased 13.6 times after receiving the second vaccine dose.
Concerns Arising From Vaccine Side Effects
An organization compiled data on adverse events reported to the Centers for Disease Control and Prevention (CDC) regarding COVID-19 vaccines, revealing that 1,605,764 people had reported adverse reactions post-vaccination as of Oct. 27, 2023. This includes 36,501 reported deaths, 20,983 heart attack cases, and 27,655 myocarditis or pericarditis cases. The vaccine has been linked to a significant number of deaths and adverse reactions, raising concerns among researchers, health care professionals, and the general public.
The Centers for Disease Control and Prevention (CDC) reported that “most patients with myocarditis or pericarditis after COVID-19 vaccination responded well to medicine and rest and felt better quickly.”
However, three scientists published a letter to the editor in the journal Clinical and Translational Discovery in February 2022. These scientists came to the conclusion, “When we vaccinate 100,000 people, we may save five lives but risk two to four deaths.”
Stuart Fischbein, a Southern California community-based obstetrician, told The Epoch Times that once you lose trust in the CDC, you start looking into everything, especially the COVID-19 vaccines. “No long-term safety studies have been conducted.” Anyone who tells a parent the vaccine is safe is making an unsubstantiated claim; the truth is, we don’t know. However, an unprecedented number of side effects have been reported. “Honestly, you’d have to be wearing blinders to not see the harm done by this vaccine,” Dr. Fischbein said.
A growing number of researchers are scrutinizing data, publishing their findings, and raising concerns about potential COVID-19 vaccine side effects. Only when people have access to accurate medical information, whether positive or negative, can trust in public health authorities and their recommended vaccination programs be restored.
Emergency Lifesaving Procedure for Cardiac Arrest
Globally, cardiac arrest kills more people than colorectal cancer, prostate cancer, breast cancer, pneumonia, HIV, influenza, car accidents, house fires, and firearms combined. Notably, the mortality rate for cardiac arrest is greater than 90%.
Previous research on cardiac arrest has discovered symptoms such as chest pain, dyspnea (breathing difficulty), lightheadedness, palpitations, and fainting. However, no effective methods for predicting or preventing this potentially fatal condition have been discovered. Approximately half of patients report symptoms in the hours, days, or weeks preceding cardiac arrest. Some people even contact health care providers a week before having a cardiac arrest, but unfortunately, most patients and their families do not act on these early warning signs. Those who call 911 before collapsing have a fivefold higher chance of survival from cardiac arrest.
According to the American Heart Association’s 2023 Heart Disease and Stroke Statistics, 40.2 percent of out-of-hospital cardiac arrest cases received CPR from bystanders. Out-of-hospital cardiac arrest occurs most frequently in homes or residences (73.4%), followed by public places (16.3%) and nursing homes (10.3%).
Cardiopulmonary resuscitation is a life-saving procedure performed in an emergency when the heart stops beating. According to Victoria, Australia data from 2021 to 2022, when the public witnesses a cardiac arrest event, citizens administer CPR in 79 percent of cases, an increase from the previous year (2020 to 2021), when the rate was 77 percent. Notably, patients who received bystander CPR had a significantly higher survival rate of 11% compared to those who did not receive CPR, who had a 5% survival rate.
To save a life, the Australian government recommends three steps: Call (dial 911), Push (perform CPR), and Shock (use an automated external defibrillator).