Unraveling the Link Between COVID-19 and Higher Alzheimer’s Risk: Prevention Strategies
A recent comprehensive study indicated that COVID-19 virus infection increases the risk of neurodegenerative diseases.
COVID-19 has a variety of effects on the brain. According to a recent comprehensive study, COVID-19 virus infection increases the risk of neurodegenerative diseases like Alzheimer’s and causes long-term cognitive impairment.
Over 55 million people worldwide are currently living with dementia, with nearly 10 million new cases diagnosed each year. Alzheimer’s disease is the most common type of dementia, accounting for roughly 60% to 70% of all dementia cases.
Patients with Alzheimer’s disease frequently experience a variety of complications, with pneumonia infection being one of the leading causes of death.
On October 18, a study published in the Journal of Neurochemistry revealed the effect of COVID-19 on Alzheimer’s disease pathology. The SARS-CoV-2 virus, which causes COVID-19, not only causes a significant increase in inflammatory factors in the body, but it also causes amyloid protein aggregation in the cerebrospinal fluid.
Postmortem examination of COVID-19-infected individuals’ brains revealed that gliosis and immune cell accumulation are associated with axonal damage and blood-brain barrier disruption and leakage. Endothelial damage and increased capillary permeability are caused by the infection, which contributes to inflammatory diseases of the central nervous system such as Alzheimer’s disease.
Cytokine storm is thought to be a major contributor to COVID-19’s neurological complications. Patients with severe COVID-19 have an inflammatory immune response that results in the release of pro-inflammatory cytokines such as IL-6 and IL-1-beta. Increased levels of these inflammatory markers have been linked to decreased neurogenesis and hippocampal-dependent memory.
Furthermore, patients with moderate to severe COVID-19 had elevated plasma levels of glial fibrillary acidic protein (GFAP) and neurofilament light chain (NfL), indicating astrocytic and neuronal damage. Some COVID-19 neurological manifestations may be attributed in part to hippocampal injury and neuronal death, potentially resulting in long-term neurological sequelae. This includes cognitive impairment in COVID patients.
COVID-19 has also been linked to dementia progression. There is an increased risk of newly diagnosed Alzheimer’s disease within the first 360 days after the initial COVID-19 diagnosis.
Higher Risk of Alzheimer’s Disease in Older COVID-19 Patients
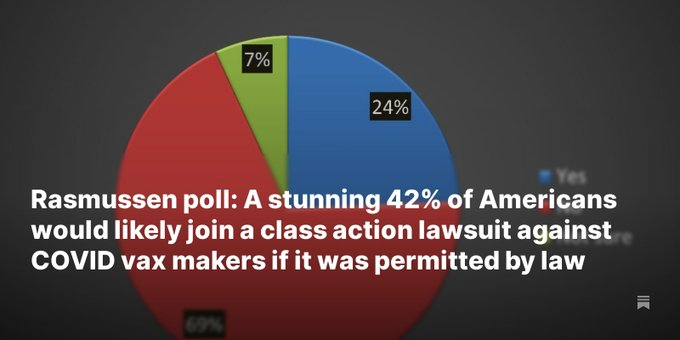
A large-scale retrospective cohort study conducted in the United States in 2022 discovered that the risk of developing Alzheimer’s disease increases significantly in older adults within a year of contracting COVID-19.
The overall risk of new Alzheimer’s disease diagnoses in the COVID-19 cohort was 0.68 percent before propensity-score matching, compared to 0.35 percent in the non-COVID-19 cohort. After propensity-score matching, the risk of new Alzheimer’s disease diagnoses increased by 69% in the COVID-19 cohort compared to the non-COVID-19 cohort. Individuals aged 85 and older, as well as females, had the highest risk of Alzheimer’s disease, with an increase of 89 percent and 82 percent, respectively.
One of the study’s authors, Dr. Pamela Davis, stated in a press release that if the number of newly diagnosed Alzheimer’s patients continues to rise, the influx of people suffering from this currently incurable disease will put a strain on long-term care resources. “Now, so many people in the United States have COVID, and the long-term effects of COVID are still being discovered.” “It’s critical to keep an eye on how this disease affects future disability,” she says.
How Can We Prevent Alzheimer’s Disease?
According to Professor Hideki Wada, a psychology professor at the International University of Health and Welfare and an eminent psychiatric expert in Japan, as the population ages and life expectancy rises, so will the number of people suffering from cognitive impairment disorders. Early detection and intervention are critical for the treatment of dementia, as they are for many other diseases.
Brain stimulation is critical for dementia prevention, and socialization is not the only way to stimulate the brain. Mr. Wada believes that learning is the most effective way to prevent Alzheimer’s disease.
In an article, Mr. Wada stated, “For those who want to do something but don’t know where to start, I recommend learning from the age of 70.” Starting to learn at the age of 70 is not about getting into a specific school, nor is it about advancing in one’s career. It is about continuing to enjoy life by learning in a stress-free and leisurely manner. He believes that learning can bring happiness, which makes it an excellent way for seniors to spend their days.
Mr. Wada also mentioned that many older people, whether in cities or rural areas, live independently. He believes that living alone is the best way to avoid Alzheimer’s disease. He went on to say that living alone keeps the brain active. In fact, everyday activities such as shopping, cooking, eating, washing dishes, taking out the trash, doing laundry, and cleaning stimulate the body, mind, and brain.
“I’m not saying that everyone should live alone. “I recommend gradually learning how to enjoy being alone for people who have strong anxiety about loneliness,” he said. He emphasized that having a positive attitude toward life is essential in later life because it is the only way to feel at ease when alone.
A person’s brain and body age naturally over time, regardless of whether they have Alzheimer’s disease. Mr. Wada suggests that we embrace an active and free-spirited lifestyle to slow the aging process. For example, one can travel to nearby towns or embark on longer journeys to sample local cuisines and indulge in delicacies such as eel. Even short day trips can introduce us to new places, providing a variety of scenery and opportunities to meet new people while inspiring us to live life to the fullest.