‘Being a Doctor and Courageous Runs in My Family’: French Scientist Behind Hydroxychloroquine Treatment for COVID-19

On February 25, 2020, Didier Raoult, a renowned French microbiologist, announced hydroxychloroquine (HCQ) as an effective cure for COVID-19. Former US President Donald Trump cited his research the following month, calling the drug a “game changer.” Dr. Raoult has since become embroiled in a worldwide controversy.
Initially, in March 2020, the Food and Drug Administration (FDA) granted an emergency use authorization (EUA) for HCQ, a drug commonly used to treat malaria and arthritis.
However, on May 22, 2020, the Lancet medical journal published a now-retracted study claiming that HCQ increased the risk of death and heart problems in COVID-19 hospitalized patients, citing data from nearly 100,000 patients in over 600 hospitals. The authors noted that the overall mortality rate was 11.1 percent, but the death rate was 16 percent or higher for the groups given various HCQ treatments—nearly double that of the control group, which did not receive HCQ treatment.
The study came before a series of health-care decisions. The World Health Organization (WHO) suspended a clinical trial of HCQ for COVID-19 in three days. During the same week, France prohibited its use on COVID-19 patients, revoking a two-week-old emergency authorization for HCQ for COVID-19.
The FDA revoked HCQ’s EUA on June 15, 2020, citing cardiac adverse events and other side effects. Six months later, the FDA approved EUAs for Pfizer-BioNTech and Moderna COVID-19 vaccines, based on “no adequate, approved, or available alternatives,” according to the FDA announcement.
“In 2006, chloroquine or hydroxychloroquine was prescribed 1 billion times.” So, if 10% of the people died from this, 100 million people would have died from heart attacks, which is ridiculous,” Dr. Raoult told The Epoch Times. HCQ is a more recent and improved form of chloroquine.
He and other experts wrote to the Lancet, claiming that the study’s findings were implausible. The journal retracted the paper a few months later. On June 4, 2020, the authors retracted the article, stating that they could “no longer vouch for the veracity of the primary data sources.” They also apologized for “any embarrassment or inconvenience” they had caused the journal and its readers.
The WHO announced the resumption of the HCQ clinical trial on COVID-19 a day before the paper was retracted. The National Institutes of Health (NIH) in the United States halted its clinical trial on June 20, 2020, citing no harm and no benefit of HCQ on COVID-19 patients. For similar reasons, the WHO discontinued its HCQ treatment arm for COVID-19 a month later. The ban on using HCQ for COVID-19 patients in France has not been lifted.
Nonetheless, Dr. Raoult continued to treat COVID-19 patients with HCQ and azithromycin, an antibiotic. On April 4, 2023, he published preliminary results from the treatment of over 30,000 patients at the Institut Hospitalo-Universitaire Méditerranée Infection (IHU), which he led until August 2022. According to him, the fatality rate of those treated with HCQ was 7%, which was “half of the fatality rate of any series of hospitalized patients [who] needed oxygen.” “So it’s very efficient,” he continued.
In May, French medical organizations called for Dr. Raoult to be sanctioned for conducting “the largest ‘unauthorised’ clinical trial ever seen.” “There is no trial,” Dr. Raoult responded, “only the doctors’ therapeutical choice.”
HCQ has remained a contentious issue over the years. Dr. Raoult, an accomplished scientist who received one of France’s highest honors—the prestigious Grand Prix Inserm—in 2010—has been labeled an anti-vaccine conspiracy theorist because he stood by his statement about HCQ’s effectiveness on COVID-19.
In response, he has stated that he is not opposed to vaccines, but that the risk-benefit equation does not hold for COVID-19 patients under 50 with low risk, particularly children, to choose to receive the injections.
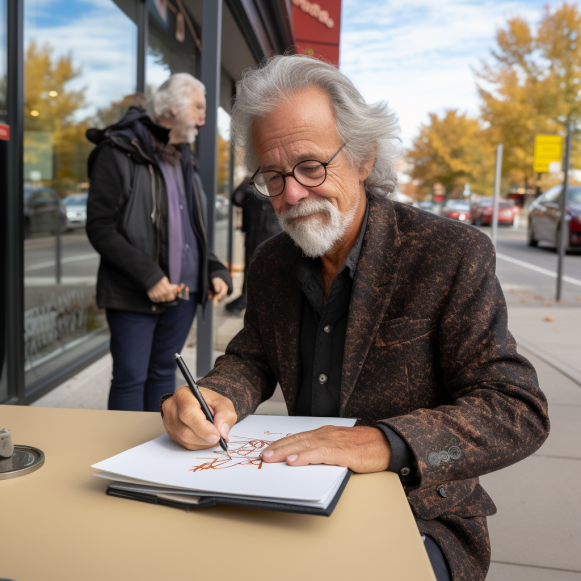
He spoke with The Epoch Times while attending a conference in Saint-Hyacinthe, a small city east of Montreal, to promote his autobiography. In France, the autobiography was released in April, and in Canada, it was released in October. “Being a doctor and courageous runs in my family,” he went on to say.
His father was a military physician, and his great-grandfather was an infectious disease specialist. He was born in French Dakar, now Senegal, in West Africa, while his father was stationed there to work on malnutrition. His grandmother ran a resistance network against the Nazis and escaped from Ravensbrück, a women’s concentration camp 50 miles north of Berlin in northern Germany.
“I don’t want to be ashamed of being less brave.” “My God, she was deported to Ravensbrück,” he exclaimed. “It runs in my family.” Sometimes you have to disobey because you believe it is wrong to obey some things that are incompatible with your moral sense.”
During the COVID lockdown, he said, patients were told not to see doctors and doctors were told not to see patients. That came across as “completely stupid” to him. In March 2020, he opened IHU to COVID-19 patients who wanted to receive HCQ treatments, and people waited in winding single-file lines outside his institute.
To him, defying the mainstream recommendation that HCQ was dangerous for COVID-19 patients was simply part of his job. “I don’t care what other people think. I’m simply describing what I’m seeing. It’s not a Christian viewpoint; I don’t have one.”
He was encouraged by a recent U.S. appeals court decision allowing three doctors’ lawsuit against the FDA to proceed. On September 1, a panel of three judges on the 5th U.S. Circuit Court of Appeals in New Orleans reopened the case, alleging that the FDA overstepped its authority by running a campaign against ivermectin’s efficacy in treating COVID-19 patients.
“It was very interesting, and I hope it happens in France someday—the doctor is in charge of treating the patient.” This is his role and responsibility. So, while the government or an agency can provide recommendations, it cannot take the place of the doctor who prescribes the treatment,” Dr. Raoult explained.
Patients, he added, should hold the doctor accountable if he fails to do his job. “But it’s not an agency that should determine what the doctor [should] do.”
The intrepid scientist, now 71, stated that he was unaware of any complaints from the 30,000 COVID-19 patients treated at IHU during his tenure. “This means that people in the Ministry of Health who have never seen the patient don’t know any better than we who have treated 30,000 people.” And I’ve been a doctor for 42 years, so I know what I’m doing.”
“Self-esteem is more important than the esteem of others,” he said about one of his autobiography’s themes. “I need to come to terms with myself.” This is essential.”