New Research Explains Why Some People Develop Fatal Blood Clots After COVID Vaccination
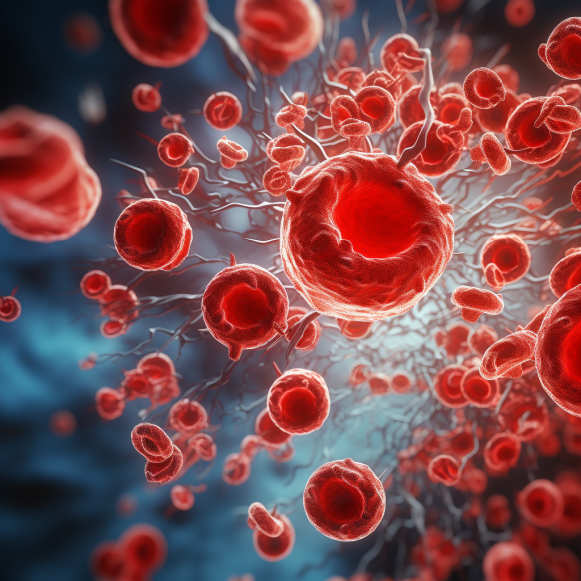
Scientists have identified a new underlying mechanism of platelet activation in vaccine-induced immune thrombocytopenia and thrombosis.
A new study may explain why some people develop a rare and often fatal blood clotting disorder after receiving the COVID-19 vaccine. Scientists from the University of Birmingham in the United Kingdom identified a new mechanism of platelet activation in vaccine-induced immune thrombocytopenia and thrombosis (VITT) in a recent study published Oct. 26 in the peer-reviewed journal Blood, funded by the National Institute for Health and Care Research and the British Heart Foundation.
VITT is a clinical syndrome caused by COVID-19 vaccines that is characterized by thrombosis (blood clots) in unusual locations and mild to severe thrombocytopenia. Thrombocytopenia is a condition in which blood platelets are abnormally low, resulting in excessive bleeding. VITT is similar to heparin-induced thrombocytopenia (HIT), but it occurs without previous exposure to the popular anticoagulant.
“Although VITT has only recently emerged, the research that it has triggered is teaching us a lot about how the body works and how it can go wrong,” said Richard Buka, co-lead author and clinical research fellow at the University of Birmingham Institute of Cardiovascular Sciences, in an email to The Epoch Times.
“Because of our ability to work on VITT, we were able to discover a previously unknown biological pathway.” This could have implications for many other fields of study, including clotting disorders in general and understanding how bone marrow produces platelets,” he added.
People with VITT or HIT, according to the study, produce antibodies against a small chemokine protein released by activated platelets and form immune complexes—large clusters of molecules that activate platelets and immune system cells, causing clotting and inflammation.
“VITT is caused by an erroneous immune response that is normally thought to protect us from infection.” Mr. Buka told The Epoch Times, “That immune response results in strong antibodies against a molecule called platelet factor 4 (PF4).” “Antibodies and PF4 form large complexes which can then activate platelets and white blood cells, leading to inflammation and blood clots.”
Although scientists were aware that PF4 is involved in innate and adaptive immunity when platelets are activated in response to infections, the precise nature of how PF4 contributes to this process was previously unknown.
Researchers collected blood samples from healthy volunteers after vaccination with AstraZeneca’s COVID-19 vaccine and nonvaccinated healthy donors for the study to determine the role of PF4 in activating platelets and causing thrombotic events.
Researchers discovered that PF4 binds to a receptor on the surface of platelets called c-Mpl, activating small cells known to cause clotting. High concentrations of PF4 have been shown to induce “robust platelet aggregation” via the c-Mpl thrombopoietin (TPO) receptor, while lower concentrations can increase platelet activation via the same pathway.
The TPO receptor is the primary regulator of megakaryocytes, which produce blood platelets.
Mr. Buka stated that he and the paper’s authors have been researching how platelets become activated in VITT. “Previously, it was thought that the antibodies themselves activated platelets, but we discovered that PF4 plays a role in this process.” “We discovered that PF4 can bind to a receptor on platelets and increase their activation, increasing the likelihood of clot formation,” he said.
Knowing what role PF4 plays in VITT could lead to better treatments, according to Mr. Buka.
“We can stop this process with ruxolitinib, a commonly used drug.” It’s reasonable to believe that this could be a good treatment for VITT, but we believe it plays a much smaller role in platelet activation. However, there are other drugs that could be used to reduce platelet activation, which would be an ideal treatment in theory,” Mr. Buka explained.
The study’s limitations include its small sample size and the various treatments received before participant samples were collected. Furthermore, due to the limited number of sera available, only a limited number of conditions were tested, and aggregation was measured over 10 minutes rather than 30 minutes for those with VITT.
“I’d really like to pay tribute to the patients and their families with VITT who have, and continue to suffer,” he said. “We are privileged to work on these extremely rare blood samples, and we will continue to strive to understand as much as we possibly can about VITT.”
AstraZeneca and Blood Clotting Disorders
After reviewing 62 cases of cerebral venous sinus thrombosis (CVST) and 24 cases of splanchnic vein thrombosis reported to the EU drug safety database EudraVigilance during the first few months of Europe’s vaccine rollout, European regulators first acknowledged a possible link between AstraZeneca’s COVID-19 vaccine and “very rare” blood clots in April 2021.
In April 2021, the UK’s vaccine regulator, the Medicines and Healthcare Products Regulatory Agency, issued a press release acknowledging that evidence of a link between AstraZeneca’s vaccine and blood clots is strong, but that more research was required.
The European Medicines Agency’s (EMA) safety committee did not recommend restricting the vaccine’s use, but it did recommend that cases of blood clotting after vaccination be listed as a possible side effect. The EMA also stated that it was looking into several reports of blood clots in recipients of the Johnson and Johnson (J&J) COVID-19 vaccine manufactured by Janssen.
Despite regulators’ insistence that the “overall benefits of the vaccine in preventing COVID-19 outweigh the risks of side effects,” more than 20 countries paused or suspended AstraZeneca use as a precaution.
In June 2021, researchers from Norway, Germany, and the United Kingdom published papers in the New England Journal of Medicine on CVST with thrombocytopenia and anti-PF4 antibodies in individuals following AstraZeneca vaccination, coining the term VITT.
Johnson & Johnson ‘Plausibly’ Related to Blood Clots, Says CDC
The J&J COVID-19 vaccine, like AstraZeneca’s, used a modified adenovirus vector rather than the mRNA technology used in Moderna and Pfizer’s COVID-19 vaccines.
In April 2021, federal agencies halted the J&J shot to investigate the vaccine’s possible link to potentially dangerous blood clots. The Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) said in a joint statement that they were investigating six cases of blood clots in women aged 18 to 48 who developed symptoms six to 13 days after vaccination in the United States.
During a meeting on April 23, 2021, the CDC’s vaccine advisors identified at least 15 women diagnosed with rare blood clots, including three who died after receiving J&J vaccination, and acknowledged that the risk of developing blood clots was highest in women aged 30 to 39.
The CDC advisory safety committee concluded that the link between blood clots and J&J’s COVID-19 vaccine was “plausible,” but that the benefits outweighed the risks. Three days later, the FDA amended the J&J vaccine’s Emergency Use Authorization (EUA) to reflect the risk of rare blood clots and said vaccinations could resume immediately. As the J&J shot became more popular, so did reports of blood clotting disorders, until the FDA revoked the shot’s EUA in June 2023 at the manufacturer’s request—for unrelated reasons.
Blood Clotting Disorders Have Been Reported Following mRNA Vaccination
Although VITT has only been publicly linked to the administration of AstraZeneca’s COVID-19 vaccine and the J&J shot, thousands of blood clotting disorders have been reported to the CDC’s Vaccine Adverse Event Reporting System (VAERS) following vaccination with Pfizer and Moderna mRNA vaccines.
According to the most recent VAERS data from the CDC, there were 48,673 reports of blood clotting disorders between December 14, 2020, and September 29, 2023. Pfizer was responsible for 33,566 of the reports, while Moderna was responsible for 11,113.
The CDC and FDA search VAERS daily for blood clotting disorders associated with vaccines, including rare thromboses (e.g., cerebral venous thrombosis), deep vein thrombosis, pulmonary thromboembolism, ischemic stroke, and myocardial infarction, according to a CDC 2021 presentation.
Using only the CDC’s inclusion criteria for blood clotting disorders, VAERS reports 19,880 cases of blood clotting disorders associated with COVID-19 vaccines, with 1,531 reports attributed to J&J, 13,748 reports attributed to Pfizer, and 4,589 reports attributed to Moderna.
Studies and case reports on blood clotting disorders following vaccination with Pfizer and Moderna’s COVID-19 vaccines were published as early as 2021.
According to an Oxford University study published in 2021, the number of people who developed CVST blood clots after COVID-19 vaccination was roughly the same for Pfizer, Moderna, and AstraZeneca. According to the study, 4 in 1 million people experienced CVST within two weeks of receiving the Pfizer or Moderna vaccine, compared to 5 in 1 million for the AstraZeneca vaccine.
Despite the fact that those infected with SARS-CoV-2 had a higher incidence of blood clots, the incidence of blood clots after vaccination was much higher than the background incidence of 0.41, indicating that vaccines pose this specific risk.
A study published in the American Journal of Hematology in February 2021 looked at thrombocytopenia after Pfizer and Moderna vaccinations. After reviewing 20 case reports of patients who developed immune thrombocytopenia after vaccination, including 17 who did not have preexisting thrombocytopenia, researchers concluded that Pfizer and Moderna’s vaccines have the potential to cause the condition and recommended additional monitoring.